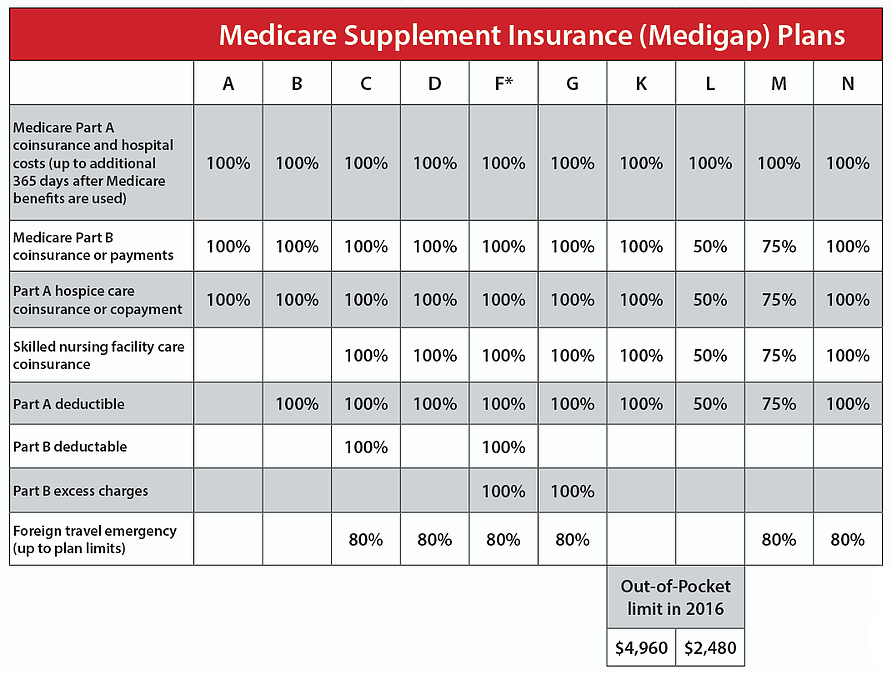
How To Check Umr Insurance Claims are administered by UMR, a division of United Healthcare, and UHC providers serve as in-network providers for participants. The prescription portion of the university's Medical Coverage Plan is administered by MedImpact. Both UHC and MedImpact offer a nationwide network of providers. Your out-of-pocket costs for eligible expenses are capped annually at $4,000 for an individual or $8,000 for a family. Refer to the coverage chart below for additional coverage details.
The district contributes to a Health Reimbursement Account for each employee who enrolls in the UMR Choice Plus Planto assist in paying a portion of your deductible. Yes, most self-fund employee health plans administered by UMR provide breast pumps and accessories as a covered benefit. The specialists at Insurance Covered Breast Pumps can help you navigate through the details of your insurance coverage policy and make sure that you get your breast pumps and supplies. Insurance Covered Breast Pumps carries all major breast pump brands to suit your unique needs and situation.
Since UMR isn't an insurance company, no drug and alcohol rehab coverage is offered directly through UMR. However, there are over 3,000 health care providers within the UMR third-party network. UMR specializes in working with each provider to expand the variety of mental health opportunities available to clients, including rehabilitation for substance abuse.
UMR recognizes the effectiveness of rehabilitation and encourages providers to offer fair coverage. For more information on getting rehab coverage, call your insurance provider. Any employee who works 30 or more hours per week during a school year or calendar year is eligible for this insurance coverage. However, participation in a Health Savings Account has some restrictions. You also cannot participate in a Health Savings Account, if you are enrolled in Medicare, receive Veteran's Administration benefits, or if you are listed as a dependent on someone else's tax return.
UMR indirectly offers health care benefits and coverage through more than 3,000 providers across the nation. Benefits and coverage depend upon the plan an employee has and what kind of health insurance an employer offers. Some plans may cost more per month, but offer more benefits when it comes to specialty substance use disorder treatment. For this reason, they are dedicated to negotiating the costs of mental health services between health care providers and members. They also understand that members need affordable coverage to receive treatment. Members can call their insurance provider to see what they cover and UMR will work to make sure the cost isn't excessive.
UMR insurance coverage generally offers a broad range of behavioral health benefits, including inpatient and outpatient drug rehab. Depending on your policy, your benefits may also extend to cover inpatient detox, IOP, and/or partial hospitalization programs. Our admissions team can verify your health insurance benefits through UMR to determine your out-of-pocket cost for rehab. You may be wondering about your UMR substance abuse treatment coverage. You don't have to worry about being denied for a substance abuse issue. The extent of coverage varies depending on the type of policy and tier level you choose.
UMR is the nation's largest third-party administrator which provides outsourced medical plan administration for companies offering self-funded plans. As such, UMR is not an insurance provider but an administrator for the medical plans offered by relatively large companies to their employees. However, as a division of UnitedHealthcare, UMR manages these medical plans in such a way that the claims process and administration of benefits are in many ways the same as a traditional insurance plan. In fact, most patients do not see much of a difference between traditional insured plans vs. a company self-funded plan admistrered by UMR.
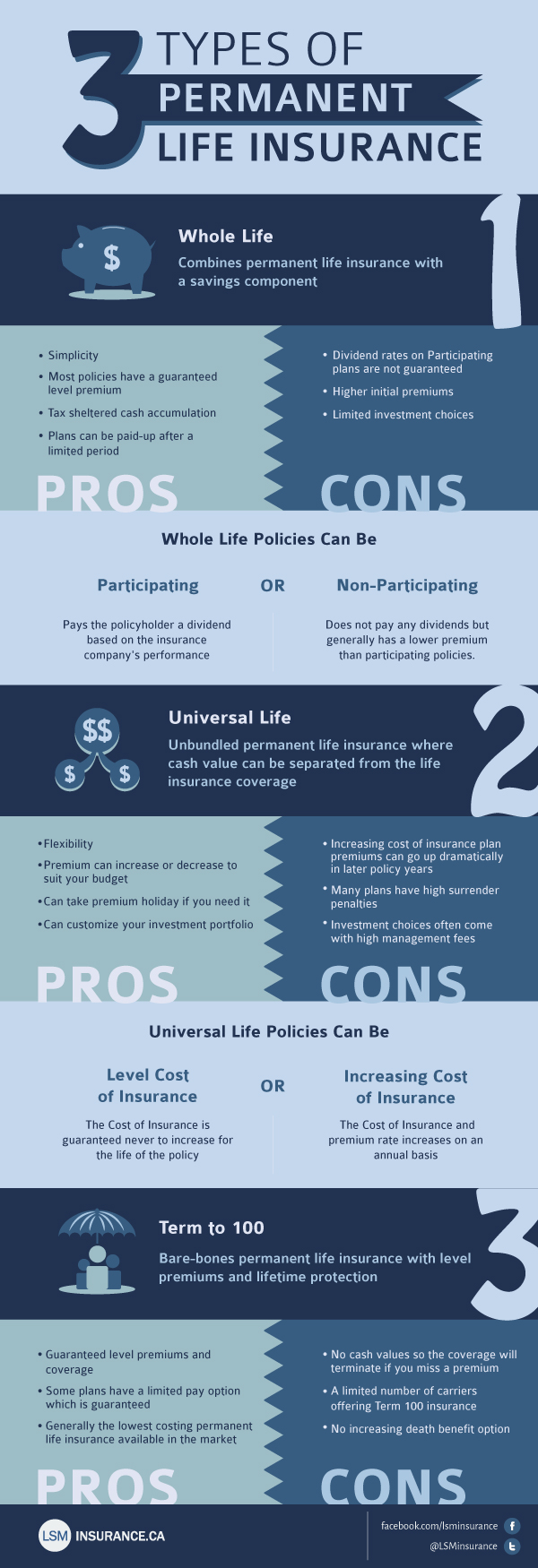
Benefit-eligible employees have the option of choosing between three health insurance plans. The only differences between our plans are the premiums, deductibles, copays and coinsurance. Unfortunately in the United States, health care isn't a given.
Yet, many employers see the benefit of providing their employees access to affordable healthcare. UMR isn't an insurance provider but helps individuals get access to the medical services they need. It's a third-party administrator hired by employers to make sure claims are paid the right way. Also, UMR ensures members receive health care services at an affordable price. UMR is a wholly owned subsidiary of UnitedHealthcare, a part of UnitedHealth Group. UMR is a third-party administrator and not an insurance company.
UMR delivers solutions for self-funded employer groups to ensure claims are paid correctly according to the member's benefit plan. UMR has a proprietary claims platform with dedicated customer service. The Health Savings Plan and Premier Plan offer coverage for out-of-network providers but your out-of-pocket expenses will be higher. When you obtain care through a non-UA-UMR provider, your benefit payments for covered services will be based on the maximum allowable payment for out-of-network services, as determined by UMR.
Charges in excess of the maximum allowable payments do not count toward meeting the deductible or meeting the limitation on your coinsurance maximum. Non-UA-UMR providers may bill you for amounts in excess of the maximum allowable payment. Prior to your medical visit, contact your insurance company to verify your benefits and coverage.
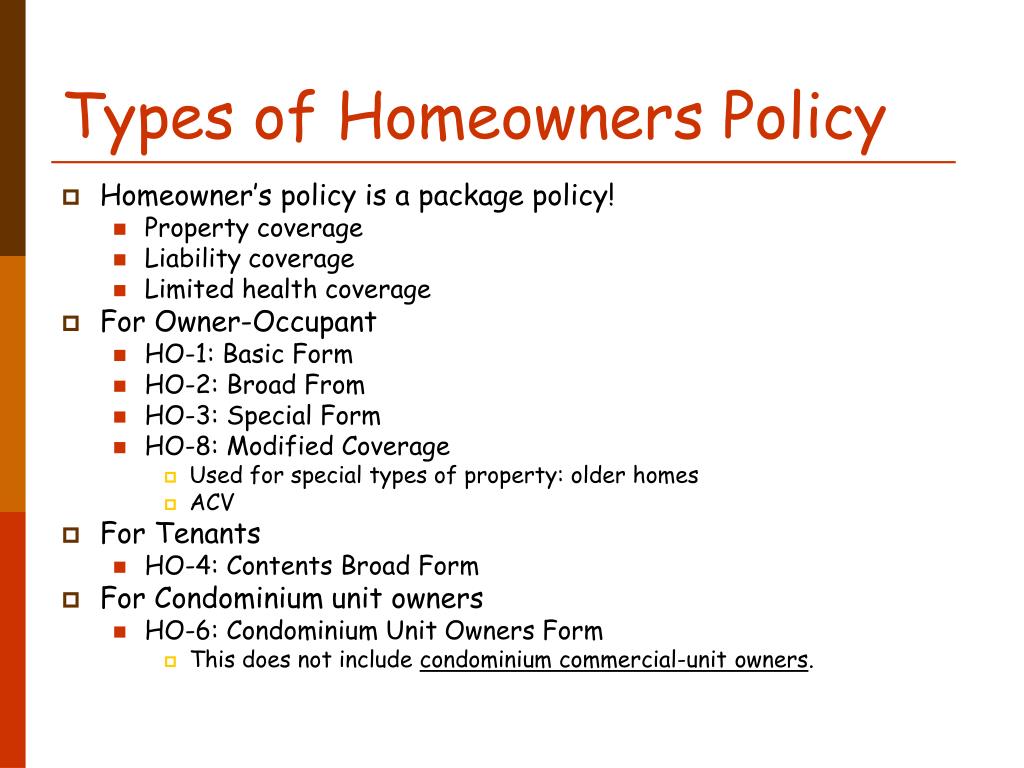
You may have network restrictions, co-payments, deductibles or other out-of-pocket expenses. Also, not all services may be covered by your insurance plan. A company that wants to give its employees healthcare benefits can choose to buy coverage from an outside insurance company or operate its own insurance plan in-house. Administering an in-house plan is a massive chore, so employers often farm out that responsibility to a specialized administrator such as United Medical Resources or UMR.
The employer provides the money, while UMR handles all the messy details that make up a health plan. Benefit payments for covered services received out of network will be based on the Maximum Allowable Payment, as determined by UMR. Charges in excess of the Maximum Allowable Payment do not count toward meeting the annual deductible or meeting the limitation on your coinsurance maximum.
Out-of-network providers may bill you for amounts in excess of the Maximum Allowable Payment. The amount of coverage you have can vary widely based on your state of residence, whether the facility is in- or out-of-network, the length of your stay, and your insurance plan level. The cost of drug and alcohol addiction treatment will vary from person to person and will also depend on the rehab center, the type of program attended, and specific services received. If an employee health care plan provides out-of-network coverage for medical and surgical benefits, they must also provide it for mental health and substance use disorders benefits.
Is a "third-party administrator" who your employer hires to ensure your claims are paid correctly, which keeps health care costs low for you and your family. UMR is not a health insurance company — they are a part of United Health Care . You should still use your medical administrator's website for viewing an explanation of benefits , requesting ID cards and other resources. You can access your medical administrator's website through the Accolade member portal.
A network is a group of doctors, labs, hospitals, specialists and other health care providers or facilities that your health care plan has contracted with to pay those providers a negotiated rate. Offering a solid benefits package is one way for companies to stay competitive in the hunt for good staff, but it can be a significant cost as well. For a company with large enough revenues, funding a health care plan in-house instead of paying premiums to an insurance company can be an attractive alternative. Insurance companies are businesses, after all, and need to make a solid profit in order to survive and thrive.
The downside is that the company also takes on the risk of unexpected expenses that could torpedo its plan. To guard against that possibility, companies often opt for a relatively inexpensive stop-loss policy that would kick in should the plan start hemorrhaging money. University of Utah Health contracts with most major health insurance carriers and transplant networks. Please call your insurance company and ask if you have access to health care services at University of Utah Health locations, and what co-payments, co-insurances, and deductibles will be your responsibility. Cleveland Clinic provides virtual visits for your convenience and health. In order to fully understand your benefits and potential cost, contact your insurance company and ask if virtual visits are included in your plan and if not, what it may cost you.
So, UMR may not be able to fully cover individuals who want to attend a substance use disorder treatment facility with luxury features. Or potential members of a facility may not be able to use certain amenities. Instead, it has guidelines that help minimize the cost of essential mental health services. Before using the mail order pharmacy, be sure to compare the costs of your prescriptions through the mail order pharmacy and your local pharmacy. We encourage you to purchase your prescriptions where you find the "best deal."Under our medical plan, you will pay the cost of the prescription until your deductible is satisfied.
The Health Savings Account is available to help pay for your medical expenses, including prescription drugs. Self-funded health insurance plans are typically used when there is no employer contribution towards employee benefits or if the company does not wish to contribute toward its employees' healthcare needs. You can use the account for yourself and any dependents who qualify as dependents on your federal income tax return. To make things even easier, you pay for services directly with a convenient Healthcare Card, which works like a debit card and allows you to pay for eligible expenses at the point of service.
Companies that provide outsourced medical plan administration are referred to as third-party administrators, and that's what UMR is. Your employer doesn't need to keep an in-house team trained and up to speed on all the legal issues involved in healthcare or to get involved in the claims process. UMR provides all that expertise, as well as the people and resources to manage the plan at a negotiated cost to your employer. It's important to understand, though, that UMR isn't an insurance company as such. Your employer puts its own resources on the line to act as the insurer. Annual physicals or OB/GYN exams and well-baby visits are covered at 100%.
Additionally, employees can participate in a weight loss program called Real Appeal . This program is free to participants of our Health Plans and uses small doable steps to help participants lose weight and reduce their risk of developing diabetes and cardiovascular disease. Be sure to understand your insurance benefits, obtain proper authorization for services and submit referral claim forms, if needed.
Many insurance plans require patients to pay a co-payment or deductible amount. Please come to your appointment prepared to make your co-payment. Before you visit us for care, it's important to understand the health insurance coverage you have and how much you'll pay – you may be able to save money by seeing an in-network provider, for example. If you have UMR as your insurance claims processor, you are most likely covered for drug and alcohol rehab. Depending on your insurance policy, your benefits may cover all or a portion of the cost of treatment at Nova Recovery Center.
If you are in need of quality chiropractic care but you are unsure of your healthcare plans guidelines when it comes to visiting a chiropractor for your condition UMR insurance can clear things up for you. If chiropractic care is included either in the original plan or as an extra add on by your employer the UMR is key. Zero Card is available to participants in both UMR Plan options at no additional premium cost. Say goodbye to deductibles, copays and coinsurance when you use the Zero Card to obtain dozens of covered non-emergency surgical procedures and medical services. It doesn't require large employee health care benefit plans to completely cover mental health and substance use disorder benefits.
It just requires equal treatment between those who suffer from them and those who don't. We are a health insurance company that acts as a broker for a select variety of health insurance plans and carriers. This site does not contain a complete list of all plans or products available. UMR is a branch of UnitedHealthcare and a third-party administrator that manages claims for other companies. Many families and individuals with this type of insurance coverage have access to affordable drug and alcohol rehab, but since insurance can be confusing, many people don't get the help they need.
UMR insurance is a third-party administrator that works with your employers insurance choice. They can administer and implement retirement plans, insurance plans, insurance add-ons, and risk management. They take some of the hassle out of providing quality insurance to employees. Managed health care also means that in some cases care can be more personalized, depending on the employer and plan.
Helping patients understand how insurance plans and healthcare benefits affect care access and costs. While UMR does not directly offer treatment coverage as they are not an insurance company, their network of healthcare providers do. Our residential programs are likely covered indirectly through UMR. A residential program is when a member lives at a facility such as ours. It's a good option because it's one of the most intense forms of treatment and UMR might be able to work with your health insurance provider to cover the bulk of the cost.
Residential treatment allows members to completely focus on recovery without external triggers. But UMR understands the rights that people with a mental health disorder and/or substance use disorder have. That way, UMR can sort it out with insurance providers if an issue surrounding coverage emerges.
Sana Lake Behavioral Wellness Center believes that every member should have the right to receive the best treatment without going into serious debt. It is also important to note that UMR provides its clients with certain discounts on in-network health services with United Healthcare's PPO Network is utilized. They also offer more than 100 other partner networks that employer insurance plans can utilize. Contract negotiations between insurance companies and providers are very common. You'll pay less when you get care in-network because your deductible, copays and coinsurance are lower than if you visit out-of-network providers.
While you have the freedom to see any licensed provider, non-network providers can bill you for amounts over R&C , and those amounts do not apply to your out-of-pocket maximum. As a third-party administrator, UMR is not an insurance company . UMR helps employers by making sure claims are paid correctly and working to minimize health care costs. Deductible– the amount you pay for covered health services before your insurance plan starts to share in the costs. If you have a $2,000 calendar-year deductible, you'll pay 100 percent of your medical bills until the amount you've paid reaches $2,000.
The length of UMR drug treatment is between you and your admissions navigator. They will provide a recommendation about what treatment program will be most helpful for your situation and how long it will take. The amount of time your UMR benefits will cover varies depending on what type of policy you have. The NIDA recommends a minimum of 3 months for substance abuse issues.6You can call the number on the back of your card or look up your plan information to find more information.




















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.